Dehydration and treatment
Contents
Causes
Symptoms
Exams and Tests
Treatment
Outlook (Prognosis)
Possible Complications
When to Contact a Medical Professional
Prevention
Dehydration means your body does not have as much water and fluids as it should.
Dehydration can be mild, moderate, or severe based on how much of the body's fluid is lost or not replenished. When it is severe, dehydration is a life-threatening emergency.
Causes
Dehydration can be caused by losing too much fluid, not drinking enough water or fluids, or both.
Your body may lose too much fluids from:
-
Excessive sweating (for example, from exercise)
-
Excessive urine output, such as with uncontrolled diabetes or diuretic use
-
Fever
-
Vomiting or diarrhea
You might not drink enough fluids because of:
-
Loss of appetite due to illness
-
Nausea
-
Sore throat or mouth sores
Dehydration in sick children is often a combination of refusing to eat or drink anything and losing fluid from vomiting, diarrhea, or fever.
Infants and children are more likely to become dehydrated than adults because they weigh less and their bodies turn over water and electrolytes more quickly. The elderly and people with illnesses are also at higher risk.
Symptoms
-
Dry or sticky mouth
-
Lethargy or coma (with severe dehydration)
-
Low or no urine output; urine looks dark yellow
-
No tears
-
Sunken eyes
-
Sunken fontanelles (the soft spot on the top of the head) in an infant
You may also have vomiting, diarrhea, or the feeling that you "can't keep anything down." All of these can be causing the dehydration.
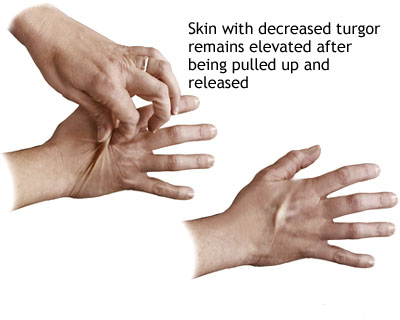
A decrease in skin turgor is indicated when the skin (on the back of the hand for an adult or on the abdomen for a child) is pulled up for a few seconds and does not return to its original state. A decrease in skin turgor is a late sign of dehydration.
A physical examination may also show signs of:
-
Blood pressure that drops when you go from lying down to standing
-
Delayed capillary refill
-
Low blood pressure
-
Poor skin turgor -- the skin may not be as elastic as normal and sag back into position slowly when the health care provider pinches it up into a fold (normally, skin springs right back into place)
-
Rapid heart rate
-
Shock
Tests include:
-
Blood chemistries (to check electrolytes, especially sodium, potassium, and bicarbonate levels)
-
Blood urea nitrogen (BUN)
-
Complete blood count (CBC)
-
Creatinine
-
Urine specific gravity
Other tests may be done to determine the cause of the dehydration (for example, blood sugar level to check fordiabetes).
Treatment
Drinking fluids is usually enough for mild dehydration. It is better to drink small amounts of fluid often (using a teaspoon or syringe for an infant or child), instead of trying to force large amounts of fluid at one time. Drinking too much fluid at once can bring on more vomiting.
Electrolyte solutions or freezer pops are very effective. These are available at pharmacies. Sports drinks contain a lot of sugar and can cause or worsen diarrhea. In infants and children, avoid using water as the primary replacement fluid.
Intravenous fluids and a hospital stay may be needed for moderate to severe dehydration. The health care provider will try to identify and then treat the cause of the dehydration.
Most cases of stomach viruses (also called viral gastroenteritis) tend to get better on their own after a few days. See also: Diarrhea
See also: Heat emergencies
Outlook (Prognosis)
When dehydration is found and treated quickly, the outcome is usually good.
Possible Complications
Untreated severe dehydration may lead to:
-
Death
-
Permanent brain damage
-
Seizures
When to Contact a Medical Professional
Call 112 if you or your child have the following symptoms:
-
Confusion
-
Dizziness
-
Lethargy
-
Light-headedness
Call your health care provider right away if you or your child has any of the following symptoms:
-
Blood in the stool or vomit
-
Diarrhea or vomiting (in infants less than 2 months old)
-
Dry mouth or dry eyes
-
Dry skin that sags back into position slowly when pinched up into a fold
-
Fast-beating heart
-
Listlessness and inactiveness
-
Little or no urine output for 8 hours
-
No tears
-
Sunken eyes
-
Sunken soft spot on the top of your infant's head
Call your health care provider if you are not sure whether you are giving your child enough fluids.
Also call your health care provider if:
-
You or your child cannot keep down fluids during an illness
-
Vomiting has been going on for longer than 24 hours in an adult or longer than 12 hours in a child
-
Diarrhea has lasted longer than 5 days in an adult or child
-
Your infant or child is much less active than usual or is irritable
-
You or your child is urinating much more than normal, especially if there is a family history of diabetes or you are taking diuretics
Prevention
Even when you are healthy, drink plenty of fluids every day. Drink more when the weather is hot or you are exercising.
Carefully monitor someone who is ill, especially an infant, child, or older adult. If you believe that the person is getting dehydrated, call your health care provider before the person becomes dehydrated. Begin fluid replacement as soon as vomiting and diarrhea start -- DO NOT wait for signs of dehydration.
Always encourage a person who is sick to drink fluids. Remember that fluid needs are greater with a fever, vomiting, or diarrhea. The easiest signs to monitor are urine output (there should be frequent wet diapers or trips to the bathroom), saliva in the mouth, and tears when crying.


 Общие симптомы
Общие симптомы  Голова, зрение, слух, речь
Голова, зрение, слух, речь  Шея и горло
Шея и горло  Грудь, сердце и дыхание
Грудь, сердце и дыхание  Живот, желудок, кишечник
Живот, желудок, кишечник  Конечности, суставы, спина, поясница
Конечности, суставы, спина, поясница  Таз, мочеполовые органы
Таз, мочеполовые органы  Наружные поверхности, кожа, волосы
Наружные поверхности, кожа, волосы