Arthritis
Arthritis is inflammation of one or more joints. A joint is the area where 2 bones meet. There are more than 100 different types of arthritis.
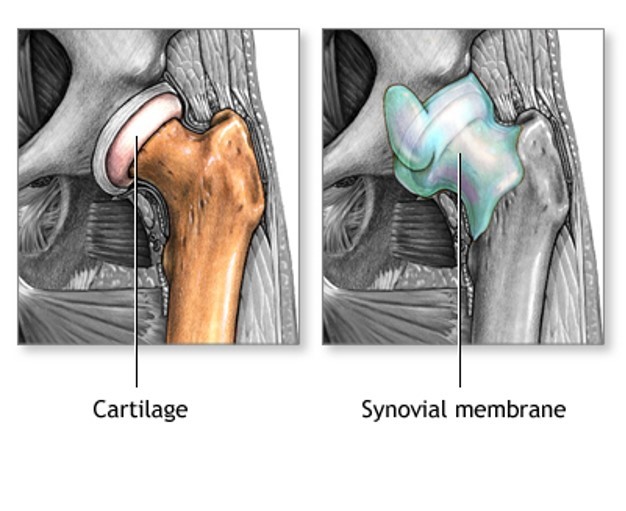
Arthritis involves the breakdown of cartilage. Normal cartilage protects a joint and allows it to move smoothly. Cartilage also absorbs shock when pressure is placed on the joint, such as when you walk. Without the normal amount of cartilage, the bones rub together. This causes swelling (inflammation), and stiffness.
Joint inflammation and damage may result from:
- An autoimmune disease (the body's immune system mistakenly attacks healthy tissue)
- Broken bone
- General "wear and tear" on joints
- Infection, most often by bacteria or virus
- Crystals such as uric acid or calcium pyrophosphate dihydrate
In most cases, the joint inflammation goes away after the cause goes away or is treated. Sometimes, it does not. When this happens, you have long-term (chronic) arthritis.
Arthritis may occur in men or women. Osteoarthritis is the most common type.
Other, more common types of inflammatory arthritis include:
- Ankylosing spondylitis
- Crystal arthritis, gout, calcium pyrophosphate deposition disease
- Juvenile rheumatoid arthritis (in children)
- Bacterial infections
- Psoriatic arthritis
- Reactive arthritis
- Rheumatoid arthritis (in adults)
- Scleroderma
- Systemic lupus erythematosus (SLE)
Symptoms
Arthritis causes joint pain, swelling, stiffness, and limited movement. Symptoms can include:
- Joint pain
- Joint swelling
- Reduced ability to move the joint
- Redness and warmth of the skin around a joint
- Joint stiffness, especially in the morning
Exams and Tests
The health care provider will perform a physical exam and ask about your medical history.
The physical exam may show:
- Fluid around a joint
- Warm, red, tender joints
- Difficulty moving a joint (called "limited range of motion")
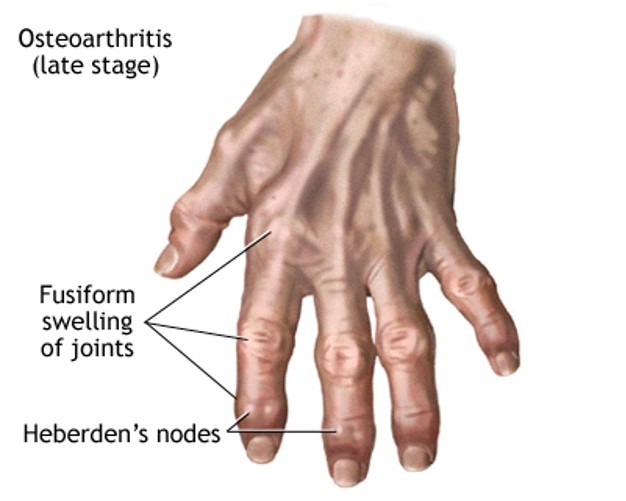
Some types of arthritis may cause joint deformity. This may be a sign of severe, untreated rheumatoid arthritis.
Blood tests and joint x-rays are often done to check for infection and other causes of arthritis.
The provider may also remove a sample of joint fluid with a needle and send it to a lab to be checked.
Treatment
The goal of treatment is to reduce pain, improve function, and prevent further joint damage. The underlying cause often cannot be cured.
LIFESTYLE CHANGES
Lifestyle changes are the preferred treatment for osteoarthritis and other types of joint swelling. Exercise can help relieve stiffness, reduce pain and fatigue, and improve muscle and bone strength. Your health care team can help you design an exercise program that is best for you.
Exercise programs may include:
- Low-impact aerobic activity (also called endurance exercise). Walking is a good example.
- Range of motion exercises for flexibility.
- Strength training for muscle tone.
Your provider may suggest physical therapy. This might include:
- Heat or ice
- Splints or orthotics to support joints and help improve their position; this is often needed for rheumatoid arthritis
- Water therapy
- Massage
Other things you can do include:
- Get plenty of sleep. Sleeping 8 to 10 hours a night and taking naps during the day can help you recover from a flare-up more quickly, and may even help prevent flare-ups.
- Avoid staying in one position for too long.
- Avoid positions or movements that place extra stress on your sore joints.
- Change your home to make activities easier. For example, install grab bars in the shower, the tub, and near the toilet.
- Try stress-reducing activities, such as meditation, yoga, or tai chi.
- Eat a healthy diet full of fruits and vegetables, which contain important vitamins and minerals, especially vitamin E.
- Eat foods rich in omega-3 fatty acids, such as cold water fish (salmon, mackerel, and herring), flaxseed, rapeseed (canola) oil, soybeans, soybean oil, pumpkin seeds, and walnuts.
- Avoid excessive alcohol and smoking.
- Apply capsaicin cream over your painful joints. You may feel improvement after applying the cream for 3 to 7 days.
- Lose weight, if you are overweight. Weight loss can greatly improve joint pain in the legs and feet.
MEDICINES
Medicines may be prescribed along with lifestyle changes. All medicines have some risks. You should be closely followed by a doctor when taking arthritis medicines.
Over-the-counter medicines:
- Acetaminophen (Tylenol) is often the first medicine tried. Take up to 3,000 mg a day (2 arthritis-strength Tylenol every 8 hours). To prevent damage to your liver, do not take more than the recommended dose. Since multiple medicines are available without a prescription that also contain acetaminophen, you will need to include them in the 3,000 mg per day maximum. Also, avoid alcohol when taking acetaminophen.
- Aspirin, ibuprofen, or naproxen are nonsteroidal anti-inflammatory drugs (NSAIDs) that can relieve arthritis pain. However, they can carry risks when used for a long time. Possible side effects include heart attack, stroke, stomach ulcers, bleeding from the digestive tract, and kidney damage.
- Prescription medicines:
- Corticosteroids ("steroids") help reduce inflammation. They may be injected into painful joints or given by mouth.
- Disease-modifying anti-rheumatic drugs (DMARDs) are used to treat autoimmune arthritis. They include methotrexate, sulfasalazine, hydroxychloroquine, and leflunomide.
- Biologics are used for the treatment of autoimmune arthritis especially rheumatoid arthritis (RA). They include etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira), abatacept (Orencia), rituximab (Rituxan), golimumab (Simponi), certolizumab (Cimzia), and tocilizumab (Actemra). These drugs can improve the quality of life for many people, but can have serious side effects.
- Other drugs for RA -- Janus kinase inhibitor: Tofacitinib (Xeljanz). This is a medicine taken by mouth that is now approved for treating RA.
- For gout, allopurinol (Zyloprim), febuxostat (Uloric) or probenecid (Benemid) may be used to lower uric acid.
It is very important to take your medicines as directed by your provider. If you are having problems doing so (for example, because of side effects), you should talk to your provider. Also make sure your provider knows about your all the medicines you are taking, including vitamins and supplements bought without a prescription.
SURGERY AND OTHER TREATMENTS
In some cases, surgery may be done if other treatments have not worked. This may include:
- Joint replacement, such as a total knee joint replacement
Outlook (Prognosis)
A few arthritis-related disorders can be completely cured with proper treatment.
Most forms of arthritis however are long-term (chronic) conditions.
Possible Complications
Complications of arthritis include:
- Long-term (chronic) pain
- Disability
- Difficulty performing daily activities
When to Contact a Medical Professional
Call your provider if:
- Your joint pain persists beyond 3 days.
- You have severe unexplained joint pain.
- The affected joint is significantly swollen.
- You have a hard time moving the joint.
- Your skin around the joint is red or hot to the touch.
- You have a fever or have lost weight unintentionally.
Prevention
Early diagnosis and treatment can help prevent joint damage. If you have a family history of arthritis, tell your provider , even if you do not have joint pain.
Avoiding excessive, repeated motions may help protect you against osteoarthritis.


 Общие симптомы
Общие симптомы  Голова, зрение, слух, речь
Голова, зрение, слух, речь  Шея и горло
Шея и горло  Грудь, сердце и дыхание
Грудь, сердце и дыхание  Живот, желудок, кишечник
Живот, желудок, кишечник  Конечности, суставы, спина, поясница
Конечности, суставы, спина, поясница  Таз, мочеполовые органы
Таз, мочеполовые органы  Наружные поверхности, кожа, волосы
Наружные поверхности, кожа, волосы